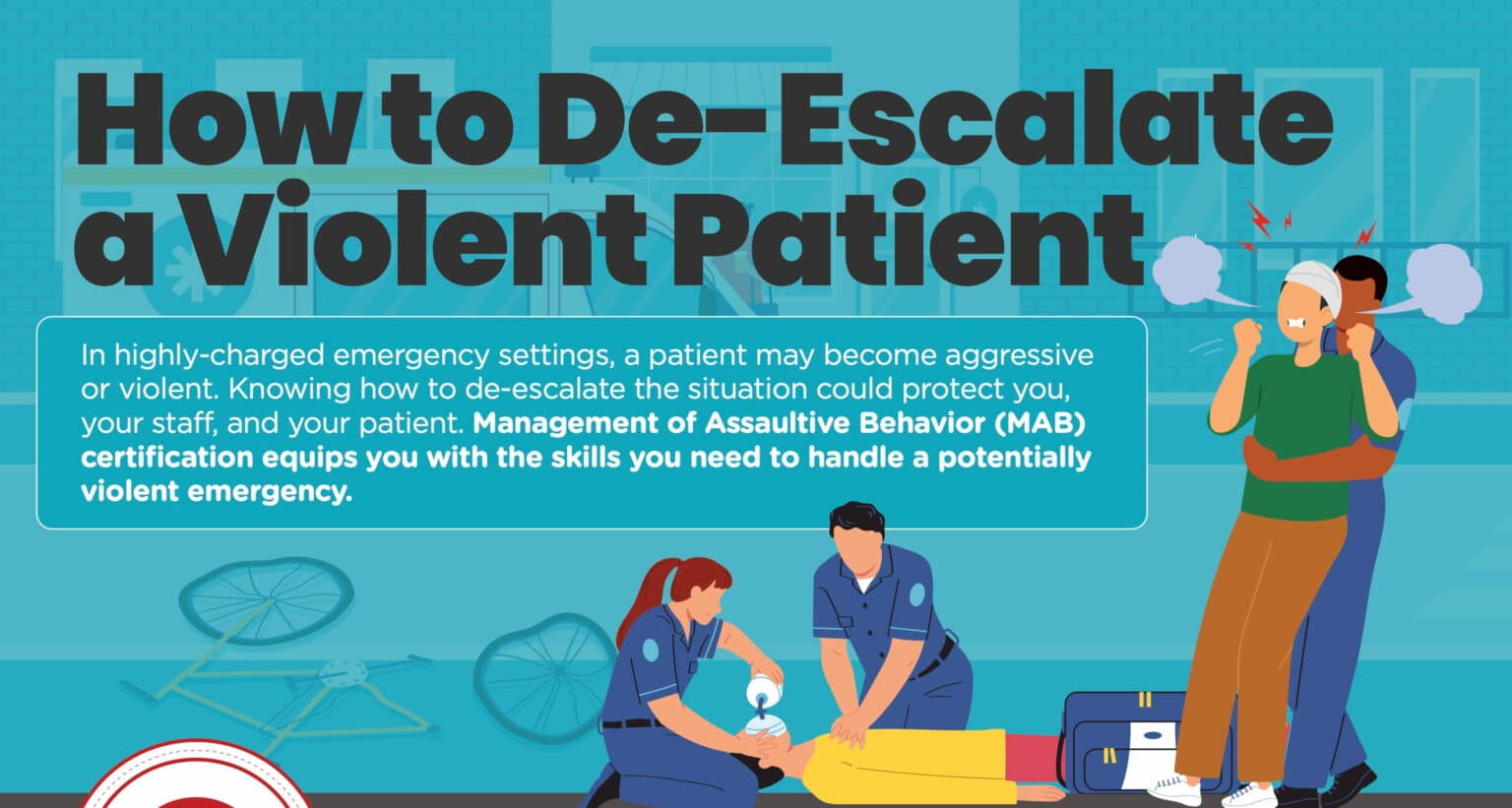
When you are dealing with a patient who is hurt and scared, situations can intensify quickly. Knowing de-escalation techniques to maintain control and restore calm keeps everyone involved safe and ensures the patient receives necessary treatment as quickly as possible.
Preparation and training is essential for effective management of assaultive behavior (MAB). It requires knowing when a situation is beginning to escalate, reasons behind the potentially violent behavior, and de-escalation steps that are both safe and within legal limits.
Understanding Assaultive Behavior
Assaultive behavior management begins with knowing what assaultive behavior is and why it might occur. The legal definition of assaultive behavior is, “violent physical actions which are likely to cause immediate physical harm or danger to an individual or others.” It might also involve a threat of property damage.
Why does a patient become potentially violent? There are numerous triggers that could lead to aggression, including:
- Pain or trauma
- Fear, stress, frustration, or anxiety
- Unmet physical or emotional needs
- Inability to communicate
- Cognitive impairment due to mental illness or substance abuse
- Feelings of powerlessness
- Not feeling heard by others
When assaultive behavior goes unchecked, it can lead to property damage or injury. It may also delay a patient from getting much needed medical care. The ability to de-escalate assaultive behavior minimizes the risk of these unwanted consequences.
The Role of De-Escalation Techniques
When emotions and tempers start to ignite, it is imperative to de-escalate the situation as quickly as possible. De-escalation techniques are not the same as intervention, which can intensify the circumstances before putting a stop to them. De-escalation involves taking control of the situation and the patient to allow for a calm resolution if possible.
Building a Foundation for De-Escalation
De-escalation techniques begin long before training on the steps takes place. To create a firm foundation for effective de-escalation, it is important to focus on the health of your staff. Emotional regulation and self-awareness are the keys to this foundation. Emotional regulation involves identifying emotions, understanding their impact, and accepting them to understand when to express them and when to take a deep breath and wait.
Regular sessions as a staff can make everyone more aware of feelings and their reactions to them. It can also help to uncover any biases and prejudices within your team that could affect how they react to different patients. An MAB course is a great opportunity to explore these topics as a team in a constructive, non-judgmental environment.
Effective De-escalation Techniques
Management of assaultive behavior involves de-escalation techniques that diffuse emotions and set boundaries while making the patient feel heard and understood. Steps include:
Active Listening and Effective Communication Strategies
Dr. George Thompson coined the phrase “verbal judo,” which illustrates the process of wrestling anger and control away from the patient in a caring and confident manner. It begins with active listening, which goes beyond hearing the patient’s words to understanding their meaning. It might include clarifying statements like, “Let me see if I understand what you are saying,” to show the patient you are truly listening to what they are saying.
Non-verbal cues and body language
Your non-verbal cues can also calm the patient while maintaining control of the situation. Proper eye contact and nodding your head shows the patient you are listening. Always keep your hands where the patient can see them to avoid frightening them, and ask them if they would like to sit down. Remain at the patient’s level, whether they choose to sit or stand, to avoid giving them an advantage in the situation.
Empathy and validation techniques
A common trigger of aggression is not feeling understood, so empathy and validation are essential to calm a patient before they become violent. Empathy involves sharing the feelings the patient is having by seeing the situation from their perspective. Validation lets your patient know their feelings are reasonable and understandable.
Distraction and redirection methods
Distraction and redirection serve to defuse emotions by directing the patient’s focus elsewhere For example, suggest you go for a walk together or offer another activity to occupy the patient.
Collaborative problem-solving and negotiation skills
It is important to let the patient know you are there to help by asking them what they need and offering to work with them to find a solution. At the same time, you can set boundaries by letting the patient know what the consequences might be if they follow through on a threat. Once you have identified the primary concern, negotiation allows for both sides to offer a solution so you can find a compromise that works for everyone.
Practical Tips for Implementing De-escalation Techniques
In addition to teaching effective de-escalation techniques, a MAB course should provide practical tips for implementing them, such as
- Assessing the situation and ensuring personal safety
- Remaining calm and composed during high-stress situations
- Avoiding power struggles and maintaining a non-confrontational approach
- Utilizing appropriate physical distance and personal space
- Seeking help and involving additional support when necessary
Training that includes role playing allows staff to rehearse these tactics so they are better prepared when a situation arises.
Training and Education for De-escalation
Emergency situations don’t arise often, which makes ongoing training and education essential to ensure your staff is always ready to address a challenging event should it arise. In addition to an initial training course for your entire team, brush-up sessions will keep the information fresh in their minds until they need it.
MAB training is essential for anyone who works in an emergency department or psychiatric ward. However, it is also helpful for first responders, nurses, and any healthcare worker that might encounter an aggressive patient.
When you are searching for an MAB course, keep in mind that the quality of instruction can vary from institution to institution. Look for a program that employs experts in the field and boasts a track record of success. If you are looking for MAB certification in your state, make sure the program you select is in compliance with your state requirements.
Ethical Considerations and Limitations
Despite your training and best efforts, there may be incidents where a patient needs to be restrained to ensure the safety of everyone involved. The use of medications and restraints is regulated by state law and compliance is mandatory. Your MAB course should go into detail about the ethical and legal limitations involved with de-escalation techniques and patient restraint.
MAB Training You Can Trust
You might not think much about de-escalation techniques until you are face-to-face with a potentially aggressive patient. Don’t be caught off guard when the situation arises. With MAB certification courses from SureFire CPR, you can rest assured you and your team will be prepared to handle any situation that comes your way.