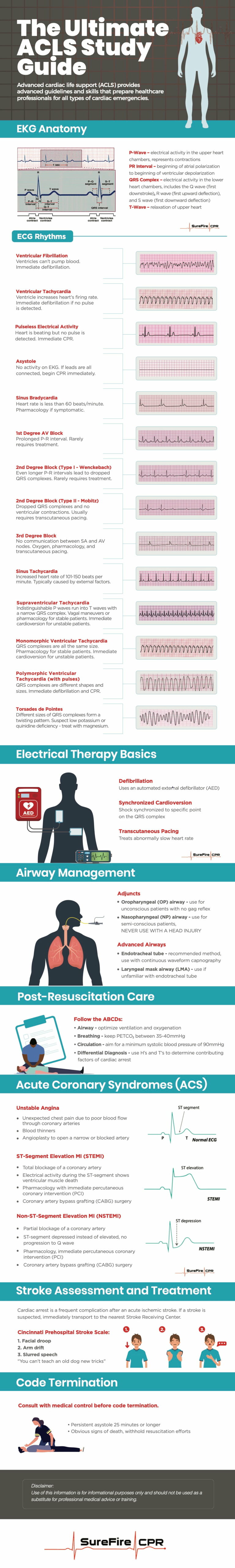
What is ACLS? Advanced cardiac life support (ACLS) teaches advanced guidelines and skills to respond to cardiovascular emergencies. It is primarily recommended for physicians, nurses, and paramedics, and teaches professionals how to respond to cardiac arrest, stroke, and other cardiac events.
This ACLS study guide is most effective for healthcare professionals that are already familiar with how to read an electrocardiogram (ECG) and administer medications. Ample practice is highly recommended prior to any ACLS training. Due to the amount of material covered in a relatively short time frame, we also advise participants to thoroughly review a pre-study guide for ACLS before taking a certification course or signing up for ACLS renewal.
The Heart Anatomy
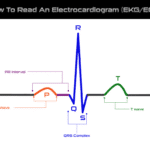
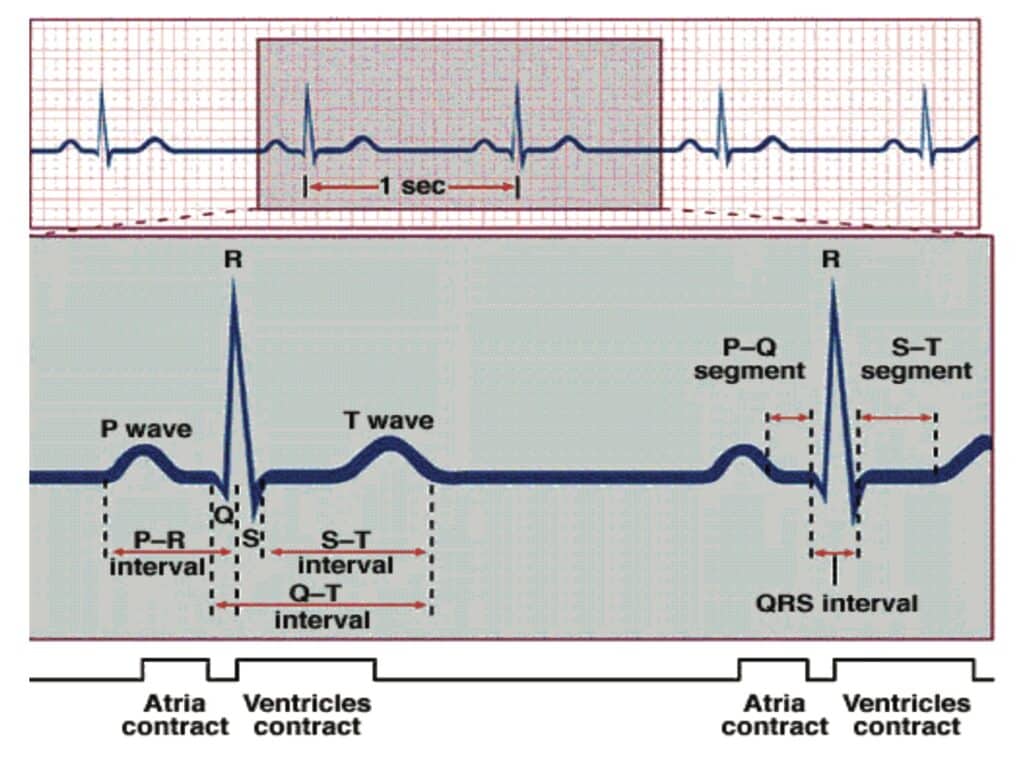
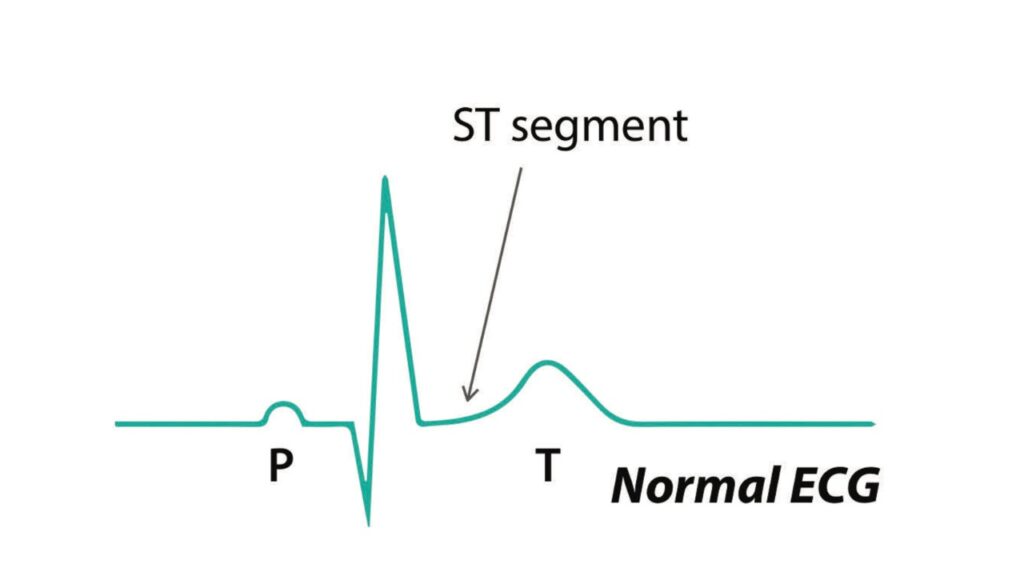
To understand various heart rhythms, it is critical to have a comprehensive understanding of heart anatomy and how electrical pathways are illustrated by an ECG.
Blood enters the heart through the atria, which sends out an electrical impulse through the sinoatrial (SA) node. The impulse travels through the atria, causing contractions that appear as P waves on an ECG.
The impulse travels from the SA node to the atrioventricular (AV) node next. The AV node sends out another electrical impulse that travels through the branches and fibers of the ventricles. Contractions caused by this impulse appear on the ECG and the QRS complex.
When the ventricles rest and repolarize, this activity registers on the ECG as a T wave. The atria also experiences a rest period, but this activity cannot be seen on an ECG.
ECG Rhythms
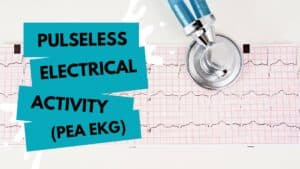
During your ACLS study, you may encounter a variety of heart rhythms, including:
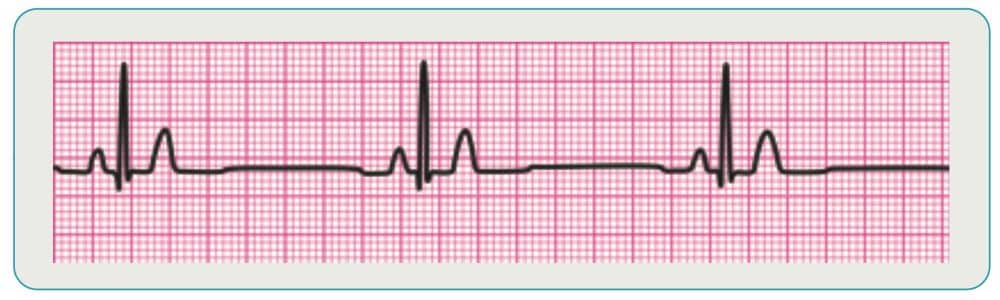
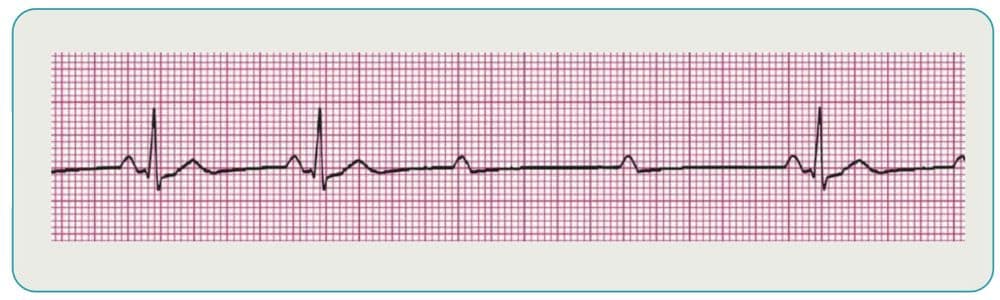
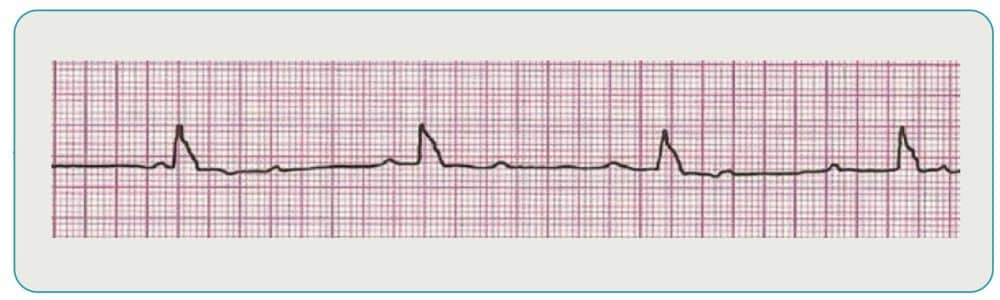
Asystole
No activity on the ECG is considered asystole, also known as “flat-lining.” Check all leads to ensure they are attached to the patient correctly and if they are, administer CPR immediately. A persistent asystole for 25 minutes or more may indicate code termination is the next step once medical control is consulted.
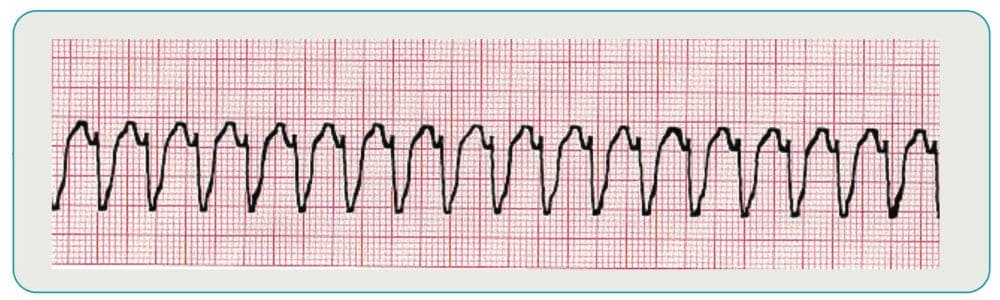
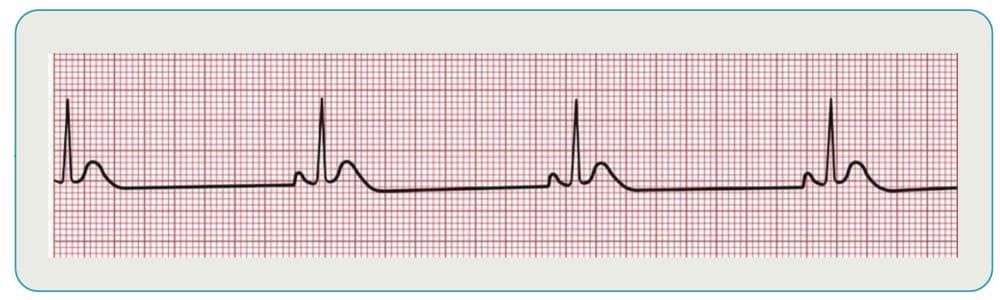
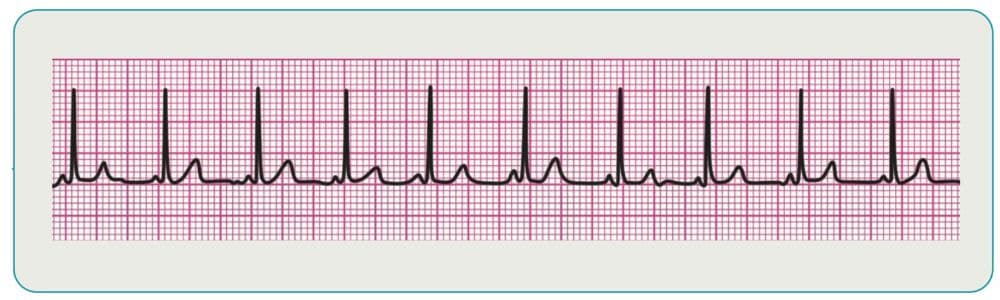
3rd Degree Block
With this type of block, there is no communication between the SA and AV nodes. Ventricles will generate their own electrical signal through an accessory pacemaker in the lower chambers. Treatment of 3rd degree block (if symptomatic) include oxygen, pharmacology, and transcutaneous pacing if necessary.
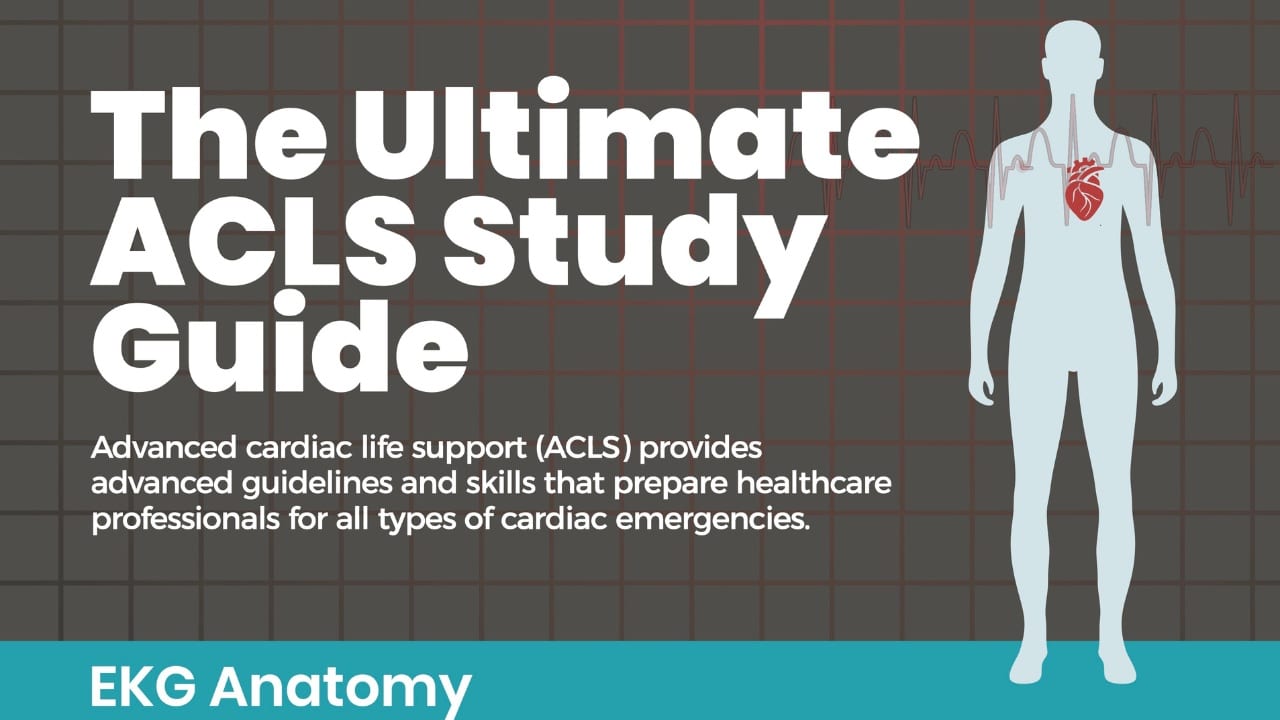
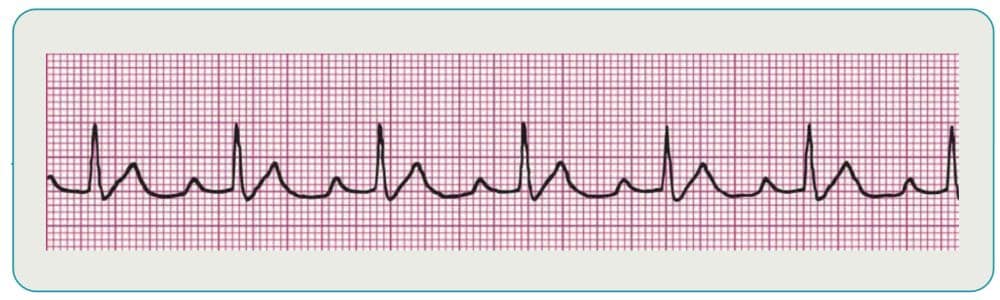
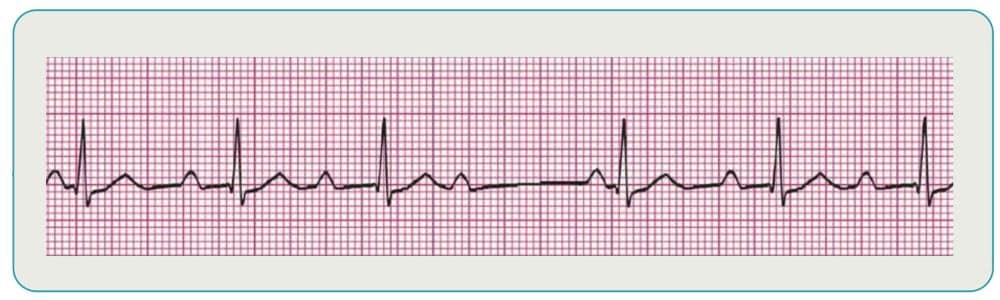
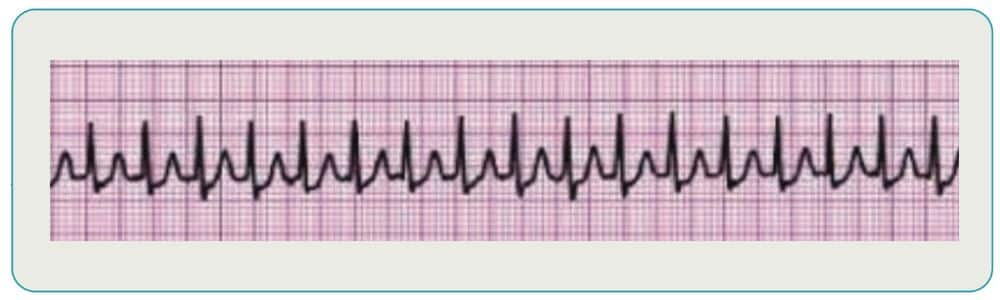
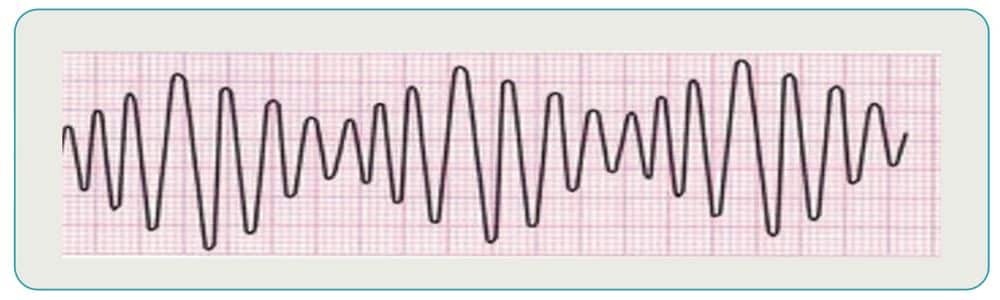
Supraventricular Tachycardia
This category of rhythms is characterized by indistinguishable P waves due to a faster rate. The rhythms also tend to have P waves that run into preceding T waves and narrow QRS complexes. Treatment of stable patients is typically vagal maneuvers or pharmacology, while unstable patients are usually candidates for cardioversion.
Supraventricular Tachycardia
This category of rhythms is characterized by indistinguishable P waves due to a faster rate. The rhythms also tend to have P waves that run into preceding T waves and narrow QRS complexes. Treatment of stable patients is typically vagal maneuvers or pharmacology, while unstable patients are usually candidates for cardioversion.
Electrical Therapy Basics
There are three ways to administer electrical therapy as part of your ACLS study guide:
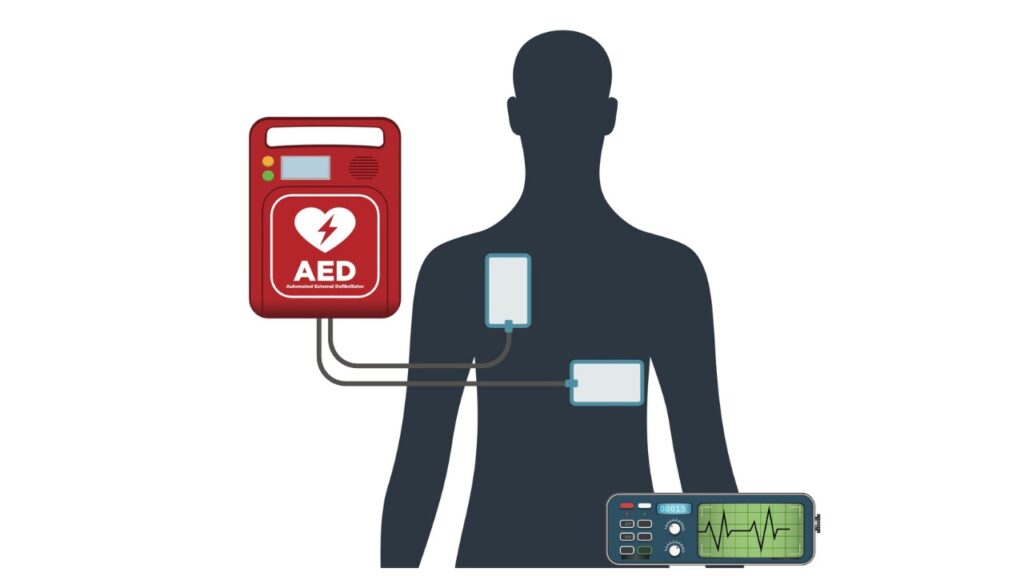
Defibrillation
An automated external defibrillator (AED) is a device that restores normal heart rhythm using a controlled electrical shock. To operate an AED, turn the device on and place the pads on the victim’s chest – 1 on the upper right side and 1 on the lower left side. The AED will analyze the heart rhythm and instruct you whether or not to shock the victim.
Synchronized Cardioversion
Synchronized cardioversion is similar to defibrillation, but delivery of the low-energy shock is synchronized to a specific point in the QRS complex. The timing is designed to prevent ventricular fibrillation as a result of the shock.
Transcutaneous Pacing
This treatment, which involves regulating heart rhythm via pads placed on the patient’s chest, can be used to address an abnormally slow heart rate. It is recommended for symptomatic patients with a heart rate of less than 60 beats per minute.
Airway Management
Airway management is another essential element of ACLS study and may be performed using adjuncts or advanced airways:
Adjuncts
These devices, which include oropharyngeal (OP) and nasopharyngeal (NP) airways, are used to access and maintain a patient’s airway. NP airways can be used for semi-conscious patients, while OP are recommended for unconscious patients with no gag reflex. Never use an NP on a patient with a head injury.
Advanced Airways
The endotracheal tube is one advanced airway that is recommended for most patients when possible. It is best to use continuous waveform capnography to monitor the placement of the endotracheal tube. The laryngeal mask airway (LMA) may be an alternative for providers who are not familiar or comfortable with using an endotracheal tube.
Once the advanced airway is in place, you should continue 100 compressions per minute without stopping for breaths. Victim should get 8-10 breaths each minute, or 1 every 6-8 seconds.
Oxygen Delivery
Oxygenation after cardiac arrest should be maintained between 94-99%, with capnography or pulse oximetry used to measure oxygenation whenever available. To maintain this level through a non-rebreather or bag valve mask, devices should be set at 10-15LPM. If using rescue breaths, they should be delivered at a rate of 1 breath every 5-6 seconds.
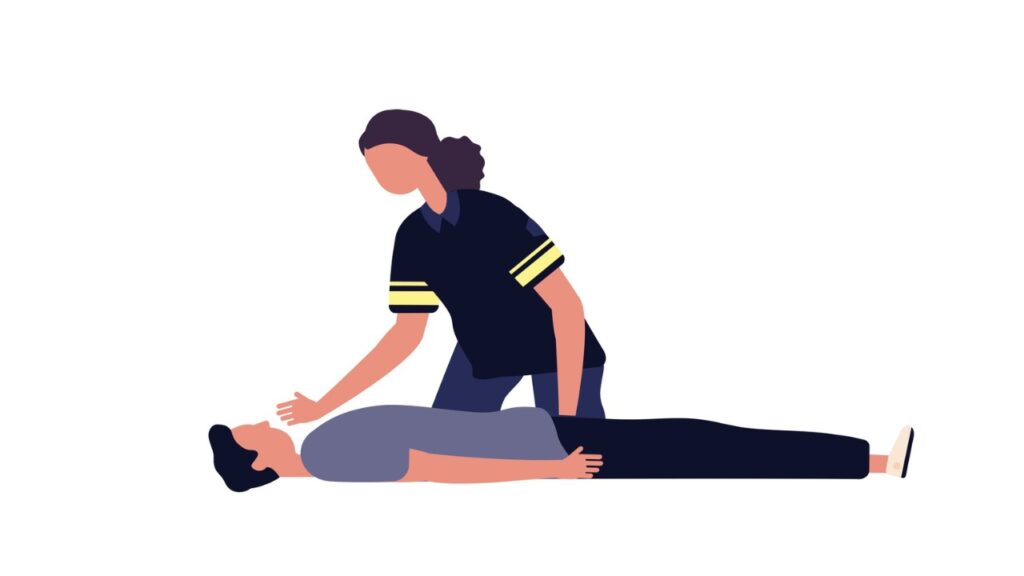
Choking Management
A choking incident can lead to reduced oxygen into the lungs and cardiac arrest if it is not treated quickly. When a victim is choking, the first priority is to raise the pressure inside the lungs so they can clear the blockage from the trachea. This is done through the Heimlich maneuver, which involves a series of powerful thrusts on the diaphragm until the blockage is expelled.
Post-Resuscitation Care
Patients may respond differently to resuscitation. While some may be awake and alert, others may remain comatose. Post-resuscitation care involves the ABCDs:
- Airway – optimize ventilation and oxygenation
- Breathing – monitor the waveform capnography to keep PETCO₂ between 35-40mmHg
- Circulation – try to achieve a minimum systolic blood pressure of 90mmHg
- Differential Diagnosis – H’s and T’s provide clues to the contributing factors of cardiac arrest
Acute Coronary Syndromes (ACS)
Acute coronary syndromes (ACS) are conditions related to a sudden decline in blood flow to the heart. Conditions might include:
Unstable Angina
Unstable angina is characterized by unexpected chest pain due to poor blood flow through the coronary arteries. Since this condition can lead to a heart attack, treatment includes the administration of blood thinners and possibly an angioplasty to open a blocked or narrowed artery.
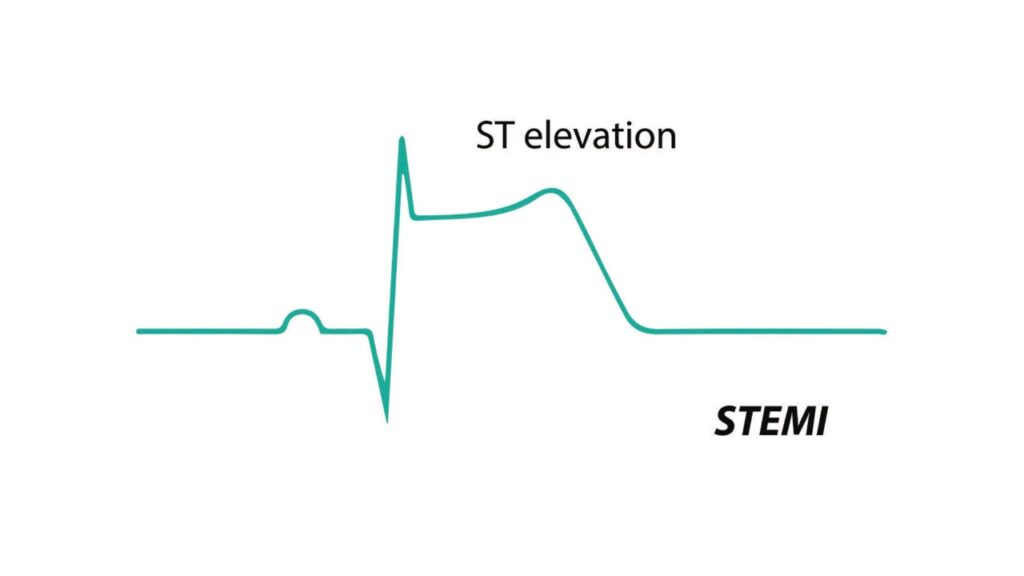
ST-Segment Elevation MI (STEMI)
This serious type of heart attack involves the total blockage of a coronary artery in the heart’s lower chambers. It can be measured in the ST-segment, which is generally seen on a EKG after the QRS complex. When there is electrical activity during the ST-segment, it indicates the muscle of the ventricles is dying, which requires urgent percutaneous coronary intervention (PCI), medications, and possible coronary artery bypass grafting (CABG) surgery.
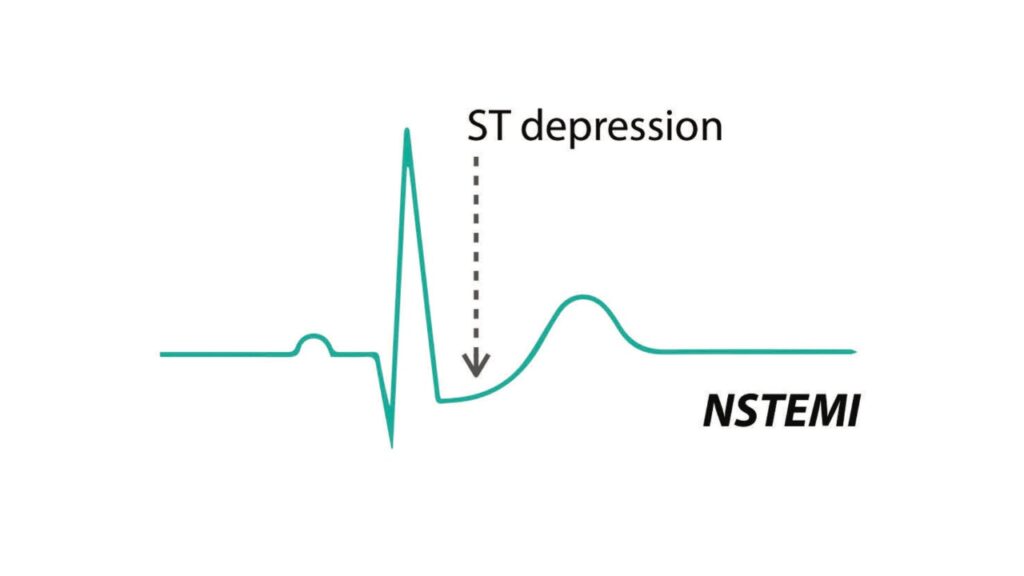
Non-ST-Segment Elevation MI (NSTEMI)
This is a heart attack that occurs due to a partial blockage of a coronary artery. While it may not cause as much heart damage as STEMI, symptoms and treatment options are similar. During NSTEMI, the ST-segment is depressed instead of elevated and there is no progression to Q wave.
Stroke Assessment and Treatment
Because cardiac arrest is a common complication after an acute ischemic stroke, stroke assessment is a critical component of an ACLS study guide. Rapid treatment is essential to minimize damage to the brain and reduce the risk for future strokes.
Symptoms of a stroke might include:
- Sudden weakness or numbness of extremities, particularly on one side only
- Loss of speech or difficulty talking
- Loss of vision, particularly in just one eye
- A sudden, severe headache
- Any of the above symptoms combined with difficulty standing or walking
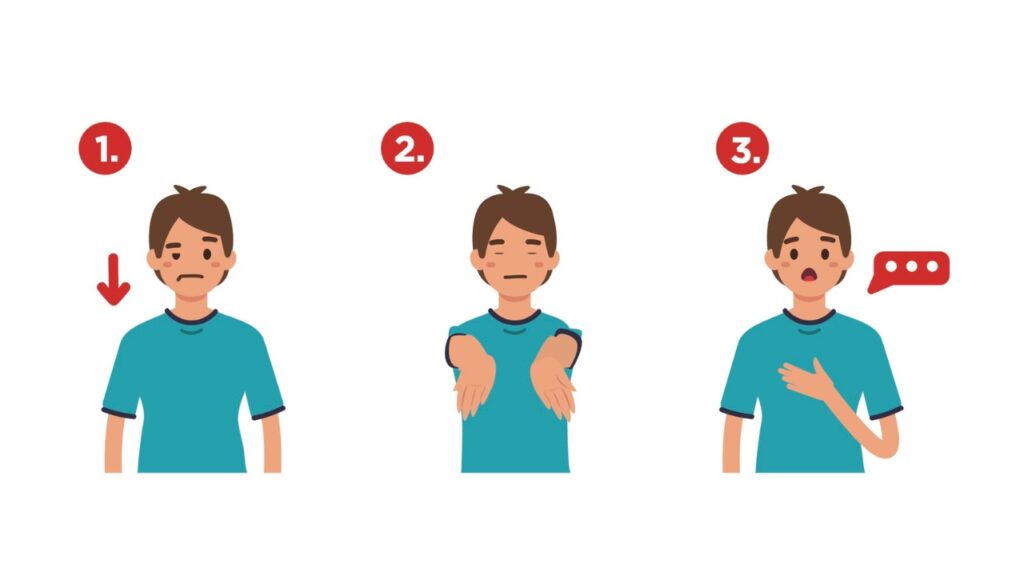
Use the Cincinnati Prehospital Stroke Scale to quickly evaluate possible stroke patients:
- Facial droop
- Arm drift
- Slurred speech – “You can’t teach an old dog new tricks”
If a stroke is suspected, immediate transport to the nearest Stroke Receiving Center is critical to reduce damage to the brain and increase survival rates.
Code Termination
When asystole has been persistent for 25 minutes or longer, despite high-quality CPR and medication, termination of resuscitation efforts should be considered. Always consult with medical control before code termination. When obvious signs of death are apparent, such as rigor mortis, withholding resuscitation efforts is the appropriate course of action.
Megacode Cases
Megacode cases involve a series of questions to evaluate your knowledge of patient assessment, diagnosis, and treatment. Megacode cases are the best way to ensure you are equipped to provide care for a patient with various cardiac complications after completing your ACLS study. Through this low-stress environment, you will be able to practice the ACLS skills you learn before you use them in a real-life situation.
ACLS Certification Prepares You for Life-Threatening Cardiac Events
Are you ready to get ACLS certified? This course will give you the knowledge you need to respond to cardiac emergencies with confidence. The team at SureFire CPR offers traditional in-person and hybrid only ACLS certification courses. The hybrid model combines online training modules, followed by a brief in-person skills check at any of our locations. We also offer recertification courses for healthcare professionals looking for ACLS renewal.
FAQ’s
What is the purpose of an ACLS study guide?
The ACLS study guide provides step-by-step instructions on how to respond to a cardiac emergency. While the ACLS course teaches all the skills necessary to treat patients in cardiac arrest, the ACLS study guide offers information reminders you might need in the event of an emergency. It should be kept with you while your certification is current for easy reference.
What does the ACLS course cover?
The ACLS course covers all the essentials of managing a cardiac emergency, including recognition and early management of cardiac arrest, airway management, ACLS pharmacology, basic life support (BLS) review, management of acute coronary syndromes and stroke, and how to work cohesively in any capacity on an ACLS resuscitation team.
What are the key components of the heart's electrical system?
The atria accepts blood into the heart initially, sending out an electrical impulse through the sinoatrial (SA) node. When the impulse arrives in the atrioventricular (AV) node, another electrical impulse is emitted that travels through the branches and fibers of the ventricles.
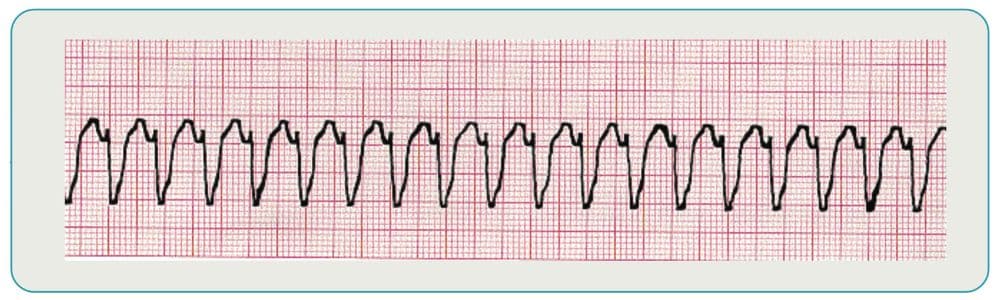
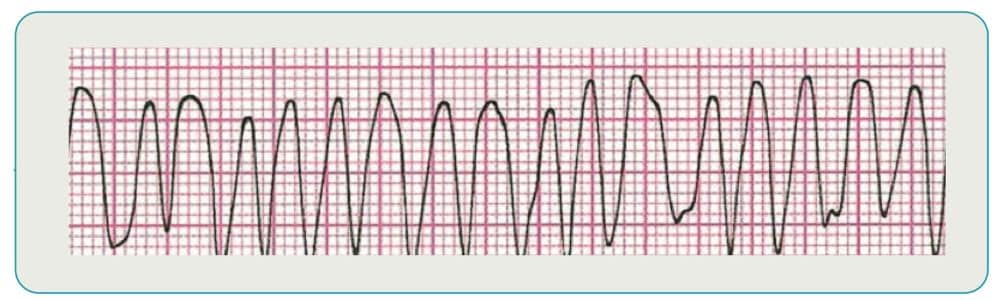
What is the recommended treatment for ventricular fibrillation?
Ventricular fibrillation is the most common type of rhythm to occur immediately after cardiac arrest. Immediate defibrillation is essential since survival chances diminish rapidly with this heart rhythm.
How do I perform synchronized cardioversion?
Sedation is usually the first step, followed by use of the defibrillator. Press the sync button and look for markers on R waves indicating “sync” mode. Press charge, announce “charge,” clear the patients and make sure there is no oxygen on the patient. If there is no conversion after the first shock, repeat the process.