Imagine your patient presents with no pulse. You begin CPR and hook the patient up to your heart rate monitor. The ECG monitor shows pulseless electrical activity (PEA). You have just minutes to restore this patient’s normal heart rhythm and electrical shock won’t be effective. What do you do?
PEA arrests are common in a hospital setting. One study found that PEA is the first documented rhythm in 30-38% of cardiac arrest patients and survival rates for those patients are poor. A critical component of ACLS must include steps to identify PEA on an EKG and respond quickly with appropriate treatment to improve outcomes for these patients.
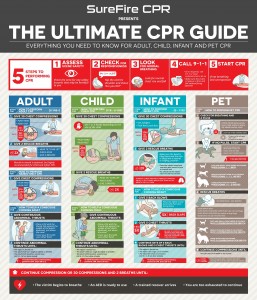
CPR and Advanced Life Support Techniques
Like any irregular heart rhythm, the first step in addressing PEA should be high-quality CPR. CPR and advanced life support techniques go hand-in-hand with any cardiac emergency. Make sure every member of your team is properly trained with ACLS and CPR certification, and keep certifications up-to-date so everyone is ready to do their part to improve patient outcomes.
What is PEA?
PEA arrest is one of the most deadly types of cardiac arrest, so every second counts when you encounter a PEA patient. With PEA, the patient has organized cardiac electrical activity, but no palpable pulse. It is a separate category from other irregular heart rhythms like ventricular tachycardia (Vtach) and ventricular fibrillation (Vfib). While it is similar to asystole in that these two rhythms are not shockable, asystole does not show cardiac electrical activity.
PEA is not considered a primary cardiac arrest. It occurs because another major organ; the vascular system, brain, or lungs, stops working properly. This prohibits blood from getting to vital organs, stopping their function. The heart is no longer receiving the oxygen it needs to function, and loss of pulse occurs. If the underlying cause of the organ failure is not identified and addressed, death is imminent.
There are two different forms of PEA:
- Pseudo-PEA – In this situation, the electrical activity within the heart may produce weak squeezing that could result in pulse detection through an arterial line, POCUS pulse check, or ETCO2. However, a palpable pulse will not be present.
- True PEA – This type of PEA features electrical activity the heart does not respond to at all. No pulse can be detected through any means.
Pseudo-PEA may be a shockable rhythm, which is why differentiating between the two can be an essential component of the diagnostic process.
Responding to PEA in Clinical Settings
There are numerous factors involved with identifying and treating PEA and every second counts when you are faced with a patient exhibiting signs of this potentially deadly heart arrhythmia. Your ability to quickly diagnose PEA by EKG and determine the specific cause is critical to the outcome of your patient. Comprehensive training in this condition is essential for any healthcare worker who might encounter cardiac events.
- Know how to identify PEA through the ECG results and whether there is a detectable pulse
- Know your Hs and Ts so you can quickly ascertain the underlying cause of PEA
- Check medical history when possible for clues to the possible cause of PEA arrest
- Monitor your PEA ECG and once a rhythm becomes shockable, be ready to shock
- Keep your team up to date on ACLS certification so you are prepared for these emergencies
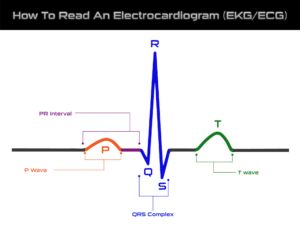
The Role of EKG/ECG in PEA Detection
Before you can treat PEA, you must identify it. Recognizing the rhythm is essential, since PEA must be addressed differently from other irregular heart rhythms. Using electrical therapy (shock) on a PEA patient won’t be effective and could actually cause more damage.
This is not the time to question how to identify PEA on an EKG. Rapid detection on the ECG and your ability to restore a shockable rhythm will impact survival odds for your patient
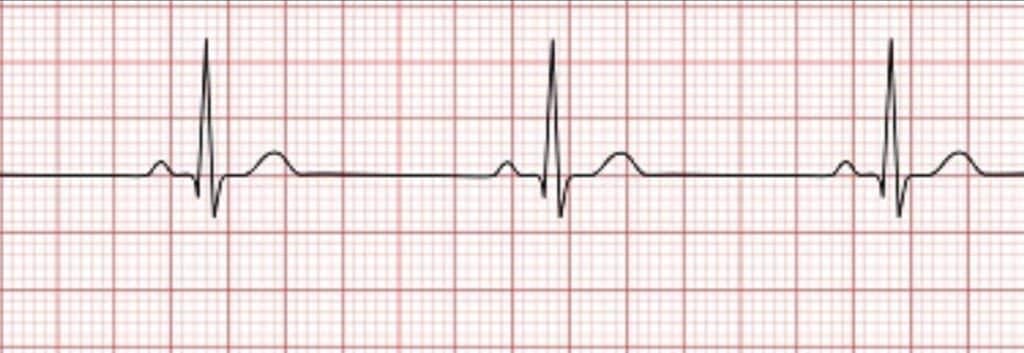
Identifying PEA on EKG
There is not a specific pattern for PEA on an ECG. In some cases, there will be a P wave, PR wave, or QRS complex. You might also detect a heart rate or no rate at all. The key factor is that there will likely be some sort of organized or semi-organized rhythm with an unresponsive patient and no pulse.
Because PEA can present in different ways, you must combine the ECG reading with an assessment of the patient, particularly pulse detection, in order to accurately diagnose this heart arrhythmia.
See ECG Rhythms in our Ultimate ACLS Study Guide.
Common Triggers of PEA
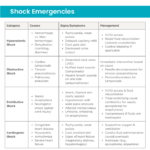
Because PEA is not a shockable rhythm, you must first identify the underlying cause of the cardiac arrest and treat it to bring the heart back to a shockable state. Diagnosing the cause of PEA involves a thorough knowledge of the Hs and Ts – a mnemonic to help you run through potential culprits as quickly as possible.
Recognizing the Culprits Behind PEA
The potential causes of PEA include 5 Hs and 5 Ts:
- Hypovolemia – loss of blood or fluid due to severe blood loss, diarrhea, vomiting, excessive sweating, and dehydration (characterized by a narrow QRS complex and rapid heart rate)
- Hypoxia – loss of oxygen (presents with a slowing heart rate and low pulse oximeter reading)
- Hydrogen ion (acidosis) – increase in hydrogen leading to low oxygen and impaired circulation (characterized by a rapid respiratory rate and low amplitude QRS complex)
- Hyper-/hypokalemia – metabolic disorders involving fluctuating potassium levels (present with irregular T waves and a widening QRS complex)
- Hypothermia – dangerously low body temperature (symptoms include shivering, drowsiness, confusion, slurred speech)
- Tension pneumothorax – air becomes trapped in the pleural space (characterized by a narrow QRS complex and rapid heart rate)
- Tamponade – fluid accumulates in the pericardium (presents with a narrow QRS complex and rapid heart rate)
- Toxins – may include pesticides, beta blockers, calcium channel blockers, benzodiazepines, opiates (symptoms will vary based on specific toxin)
- Thrombosis (pulmonary) – blockage in the primary artery of the lung (may display with narrow QRS complex and rapid heart rate)
- Thrombosis (coronary) – blockage in a coronary artery (characterized by a fast heart rate with inversions in the T waves, S-T segment changes, and possibly Q waves)
Learn more about the Hs and Ts in ACLS.
Why EKG Certification Matters
EKG certification is a credential all team members should have to ensure cardiac emergencies are quickly and accurately diagnosed, particularly cases of PEA. An EKG course teaches you all of the ins and outs of analyzing heart rhythm and rate so you can respond appropriately.
Enhancing Your Skills with SureFire CPR
Get the certification you need with SureFire CPR. Our instructors are all healthcare professionals who believe learning life-saving skills should be fast, effective, and easy. We offer CPR, ACLS, and EKG certification courses online, in-person, and on-site throughout the Southern California area. Our aim is to make courses fun and easy to follow, so you retain the knowledge you learn long after you receive your certification.
Don’t wait to get the certification you need for your career and your patients. Contact SureFire CPR or check out our current class schedule today.